Total Knee Replacement (TKR)
Total Knee Replacement performed using MAKO Robotic technology by Dr Amir Kalanie
Total knee replacement, also called total knee arthroplasty, is a surgical procedure in which the worn out or damaged surfaces of the knee joint are removed and replaced with artificial parts. The knee is made up of the femur (thigh bone), the tibia (shin bone), and patella (kneecap). The meniscus, the soft cartilage between the femur and tibia, serves as a cushion and helps absorb shock during motion. Arthritis (inflammation of the joints), injury, or other diseases of the joint can damage this protective layer of cartilage, causing extreme pain and difficulty in performing daily activities. We may recommend surgery if non-surgical treatment options have failed to relieve the symptoms.
Indications
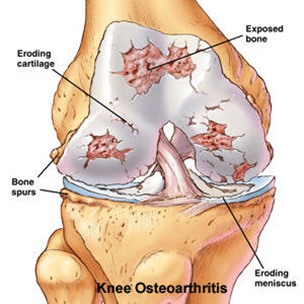
Total knee replacement surgery is commonly indicated for severe osteoarthritis of the knee. Osteoarthritis is the most common form of knee arthritis in which the joint cartilage gradually wears away. It often affects older people.
In a normal joint, articular cartilage allows for smooth movement within the joint, whereas in an arthritic knee the cartilage itself becomes thinner or completely absent. In addition, the bones become thicker around the edges of the joint and may form bony “spurs”. All of these factors can cause pain and restricted range of motion in the joint.
We may advise total knee replacement if you have:
- Severe knee pain which limits your daily activities (such as walking, getting up from a chair or climbing stairs).
- Moderate to severe pain that occurs during rest or awakens you at night.
- Chronic knee inflammation and swelling that is not relieved with rest or medications
- Failure to obtain pain relief from medications, injections, physical therapy, or other conservative treatments.
- A bow- legged knee deformity
Causes
The exact cause of osteoarthritis is not known, however there are a number of factors that are commonly associated with the onset of arthritis and may include:
- Injury or trauma to the joint
- Fractures at the knee joint
- Increased body weight
- Repetitive overuse
- Joint infection
- Inflammation of the joint
- Connective tissue disorders
Diagnosis
We will diagnose osteoarthritis based on the medical history, physical examination, and X-rays.
X-rays typically show a narrowing of the joint space in the arthritic knee.
- Our knees are vulnerable to wear and tear. Cartilage is the slippery lubricant that covers your joints and lets them glide smoothly. Over time, this cartilage can wear away, particularly in the knee and hip joints that support your body. Your age, your weight, and old injuries also matter. The result is that the bones of the joints rub against each other without enough cushioning. This is called osteoarthritis (OA).
- The first sign of knee OA is often pain and stiffness. Similar to hip OA, pain is typically worse in the morning. You may find that your knee locks or buckles when you walk. Eventually, you may feel pain and have trouble flexing your knee. Kneeling or climbing stairs may make the pain worse. The knee may feel tight and swollen, and hurt at the back of the joint.
- You can relieve OA at home. First, get enough rest. While it's important to stay active, give your joints time off when they hurt. Second, ask us about taking chondroitin and glucosamine. These supplements may help ease pain and help you move more comfortably. You can try anti-inflammatory drugs like ibuprofen (Advil, Neurofen), Diclofenac (Voltaren rapid 25, Fenac) or Naproxen sodium (Naprogesic, Naprosyn) if we say these are safe for you. Panadol Osteo is also worth a try. They can provide fast relief for mild to moderate arthritis pain.
- Viscosupplementation Hyaluronic acid injected into an arthritic joint can afford symptomatic relief of pain and stiffness in about 70% of cases provided that the OA is not bone on bone. The injections can be repeated up to 3 times for maximal effect. We currently use "Durolane" (Bioventus) which is a stabilised single injection preloaded 60ml Hyaluronic acid in 3 ml. There is some evidence that Hyaluronic acid acts to heal early cartilage lesions and slow progression of disease.
- Stem Cell Therapy Currently there is no objective evidence that the results of stem cell therapy are any better than placebo in the treatment of osteoarthritis. There is anecdotal evidence but no randomised prospective blinded studies to support this therapy. St Vincent's Bone & Joint do participate in ongoing evaluation of this therapy but accept that at this stage the treatment is experimental and requires more study.
- Losing weight reduces pain and stiffness. Being overweight puts extra stress on your knees and hips. You may be surprised to know that every 3 kg you lose can lower your arthritis pain by as much as 20% by decreasing the load in the joint.
- Exercise helps joints work better. Keep limber and start with stretching. Low-impact exercise, such as swimming or cycling, will strengthen your joints and increase their range of motion. A physio therapist can show you exercises to strengthen the muscles that support your knees or hips. Stronger muscles can reduce the stress on your joints during everyday activities, too.
- OA of the knee or hip can make it hard to walk. If there isn't enough cartilage lining your joint, walking might hurt. Your joint may get so stiff that you can't bend your knee or rotate your hip. People with severe OA of the knee or hip may need a cane to walk.
- Without treatment, OA usually gets worse. As the cartilage continues to wear away, the joint may become swollen and painful. In severe cases, bone rubs directly against bone, making any movement of the joint excruciating. Even at this point, you can still take steps to slow the damage.
- Joint replacement gets rid of pain. When other things don't provide enough relief, your GP may recommend seeing us to discuss a hip or knee replacement. Often all the joint needs replacement, which is called a total joint replacement. In certain situations, only a partial joint replacement is necessary, especially in the knee. After recovering, most people can walk more easily and are pain-free.
- Rehabilitation is vital after joint replacement surgery. A rehab program includes vigorous exercises to make sure your new joint is flexible and to strengthen the muscles around it. People who stick to their rehab program have the greatest possible range of motion, meaning they can do more of the activities they used to do. All joint replacement patients continue to improve for at least 12 months, provided they keep up an exercise programme. Recovery normally takes 3 months until you are back to doing all your regular activities without discomfort.
What medications should I stop before operation?
Many tablets can cause excessive bleeding at operation so it is essential to cease taking the medication well beforehand. However, if you are taking such medication for problems with your heart or blood vessels, please ensure you discuss this us.
Stop the following one month (30 days) prior to admission:
- HRT (excluding Prednisone)
- Tamoxifen
- Arava
- Letrozole
Stop the following 5 days prior to admission:
- Alka-Seltzer, Chemgesic, Percoden
- Asasantin, Codiphen Forte, Persantin
- A.S.A. Aspirin, Cliopidogrel, Plavix
- Aspirin, Codis, Rheumat-ese
- Aspalgin, Codox, Rhusal
- Aspro Clear, Codral Forte, Solocode
- Asprodeine Soluble, Disprin, Solvin
- Astrix, Doloxene, Solprin
- Bex, Ectorin, Salicylamide
- Bufferin, Ensalate, SRA
- Cartia, Iscover, Vincents powder/tabs
- Cardiprin, Morphalgin, Winsprin
- Clusinol, Orthoxical Cold & Flu Tablets
Anti-Inflammatory Drugs
ACT-3, Clinoril, Inza, Priohexal, Aclin, Crysanal, Mefic, Prioxicam, Actiprofen, Dinac, Methotrexate, Proxen, Advil, Doloboid, Mobic, Rafen, Arthexin, Feldene, Naprogesic, Rheumacin, Arthrotec, Fenac, Naprosyn, Surgam, Brufen, Flexin, Nurofen, Tilcotil, Bugesic, Ibuprofen, Orudis, Toradol, Candyl, Indocid, Oruvail, Tri-profen, Celebrex, Inflam, Ponstan, Voltaren
Anticoagulants
Warafin/Coumarin/Marevan cease 5 days pre-op. The tablets will have to be withdrawn prior to surgery and CLEXANE injections are substituted up to the time of operation.
ANTICOAGULANT tablets will be resumed after surgery under the direction of A/Prof Neil.
HERBAL MEDICINE
Arnika, Gingko (36 Hours), Garlic (7 Days), Ginger, Ginseng (7 Days), Saw Palmetto, Vitamin E, Echinacea, Primrose Oil, Fish Oil, Krill Oil
PANADOL, PANADEINE OR PAINKILLERS may be taken for pain relief up to the time of operation.
If you are uncertain about any of your medications please discuss this with A/Prof Neil or Dr Kalanie.
Reasons that you may benefit from TKR commonly include
- Severe knee pain that limits your everyday activities, including walking, going up and down stairs, and getting in and out of chairs. You may find it hard to walk more than a few blocks without significant pain and you may need to use a cane or walker.
- Moderate or severe knee pain while resting, either day or night.
- Chronic knee inflammation and swelling that doesn’t improve with rest or medications.
- Knee deformity – a bowing in or out of your knee.
- Failure to obtain pain relief from non-steroidal anti-inflammatory drugs. These medications, including aspirin and ibuprofen, often are most effective in the early stages of arthritis. Their effectiveness in controlling knee pain varies greatly from person to person. These drugs may become less effective for patients with severe arthritis.
- Inability to tolerate or complications from pain medications.
- Failure to substantially improve with other treatments such as cortisone injections, physical therapy, or other surgeries.
Most patients who undergo TKR are aged 60 to 80, but we evaluate patients individually. Recommendations for surgery are based on a patient’s pain and disability, not necessarily age.

We have patients as young as age 20 and older than 95 who have undergone successful TKR.
Preparing for surgery
Medical evaluation
If you decide to have TKR surgery, we may organise for you to see one of our cardiovascular physicians, with whom we work, for a complete medical assessment and to optimize your fitness for the operation. This is especially likely if you have a strong history of DVT, serious cardiac disease or are on anticoagulants or other blood thinners.
Preadmission clinic
You will attend preadmission clinic a week or 2 before your scheduled operation. At preadmission, the clinic nurse will arrange routine blood tests, urine analysis, ECG and X-rays including a chest X-ray.
You will also be seen by your anaesthetist who will discuss the anaesthetic options that are best for you, and inform you of any risks specific to you.
What to bring to the hospital?
- Nightshirts rather than pyjamas.
- Toiletries and personal items
- Loose fitting garments.
- X-rays or investigations relevant to surgery.
- Usual medications
Preparing your skin and leg
Your knee and leg should not have any skin infections or irritation. Your lower leg should not have any chronic swelling. A skin antiseptic will be given to you to use for several days before operation to clean your leg and sterilize the skin.
Contact St Vincent’s Bone & Joint prior to surgery if there are any issues with the skin of your leg to be operated.
Dental evaluation
Although the incidence of infection after TKR is very low, an infection can occur if bacteria enter your bloodstream. Treatment of significant dental disease (including tooth extractions and periodontal work) should be considered before your TKR surgery.
There should be no gum or mouth infection present prior to elective TKR.
Please also note within 3 months after joint replacement surgery patients undergoing any dental treatment will need to take 500 mg of Amoxil, 2 tablets, 2 hours before the dental work is performed and then 2 tablets after (on the same day).
This protocol is for A/Prof Michael J Neil and Dr Amir Kalanie’s patient’s. Other surgeons may have similar protocol or different so always best to speak with your treating specialist.
Procedure
The goal of total knee replacement surgery is to relieve pain and restore the alignment and function of your knee.
The surgery is performed under spinal or general anaesthesia combined with intraoperative injections of local anaesthesia, and a "Pain buster" local anaesthetic catheter which is left in the joint. In addition to this, Femoral Nerve blocks or regional anaesthesia is also added. We will make an incision in the skin over the affected knee to expose the knee joint. Then the damaged portions of the femur bone are cut at appropriate angles using specialised jigs. The femoral component is attached to the end of the femur with or without bone cement. The surgeon then cuts or shaves the damaged area of the tibia (shinbone) and the cartilage. This removes the deformed part of the bone and any bony growths, as well as creates a smooth surface on which the implants can be attached. Next, the tibial component is secured to the end of the bone with bone cement or screws. We will place a plastic piece called an articular surface between the implants to provide a smooth gliding surface for movement. This plastic insert will support the body’s weight and allow the femur to move over the tibia, similar to the original meniscus cartilage. The femur and the tibia with the new components are then put together to form the new knee joint. To make sure the patella (knee cap) glides smoothly over the new artificial knee, its rear surface is also prepared to receive a plastic component. With all the new components in place, the knee joint is tested through its range of motion. The entire joint is then irrigated and cleaned with a sterile solution. The incision is carefully closed, drains are inserted and a sterile dressing is placed over the incision.
For TKR, the implant we use is the Apex Fixed Bearing High Flexion PS Knee
(Omnisurgical/Global Orthopaedic Technology)
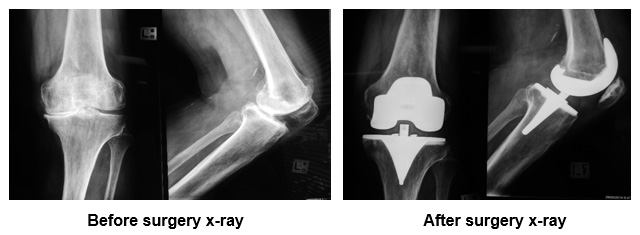

Legogram Post TKR showing perfect mechanical alignment following computer assisted surgery
Your stay in hospital
.
You will most likely stay in the hospital for 5 days for a first-time operation (“primary”), and longer for a “Revision” operation. After surgery, you will feel some pain, but medication will be given to you to make you feel as comfortable as possible. Walking and knee movements are important to your recovery and will begin immediately after your surgery.
Your knee will be iced with packs and/or “liquid ice” spray and placed on a CPM (Continuous Passive Motion”) machine post operatively to massage the leg and remove any blood within.
You will be asked to stand and walk within 24 hours of operation. Initially a frame will be used, and then you graduate to crutches or a stick.
The drains and IV lines will be removed the following day. Regular oral painkillers and anti-inflammatory are used rather than narcotic injections or PCA (” Patient Controlled Analgesia”) as we have found there is less nausea and more clear headedness this way.
As a lot of these drugs are constipating, you will be placed on a bowel care program immediately to avoid this distressing complication. To avoid lung congestion after surgery, you should breathe deeply and cough frequently to clear your lungs. To minimize the risk of clots forming, you will be mobilized rapidly, you will have TED (antiembolic) stockings applied, as well as inflatable calf compressors and a blood thinner such as Aspirin or “Clexane”.
Foot and ankle movement is encouraged immediately following surgery to also increase blood flow in your leg muscles to help prevent leg swelling and blood clots. Most patients begin exercising their knee the day after surgery. Our physiotherapists will teach you specific exercises to strengthen your leg and restore knee movement to allow walking and other normal daily activities soon after your surgery particularly concentrating on getting the knee fully straight and flat by quadriceps contraction. Bending is encouraged but not forced, and always comes once the swelling goes down. This may take 6 weeks or more.
On day 5 (planned discharge day), you will have a Doppler ultrasound scan of the operated leg performed, looking for clots. Your dressing will be changed if you are going home, but will be changed in rehabilitation if you are being transferred.
You will usually mobilise onto crutches fully weight bearing for discharge. Crutches or a stick are to be used outdoors for at least 6 weeks or until review by us.
Post-operative care
Rehabilitation begins immediately following the surgery. A physical therapist will teach you specific exercises to strengthen your leg and restore knee movement. Knee immobilizers are used to stabilise the knee. You will be able to walk with crutches or a walker. A continuous passive motion (CPM) machine can be used to move the knee joint. Continuous passive motion is a device attached to the treated leg which constantly moves the joint through a controlled range of motion, while the patient relaxes. Your physical therapist will also provide you with a home exercise program to strengthen thigh and calf muscles.
Risks and complications
As with any major surgery, possible risks and complications associated with total knee replacement surgery include:
- Knee stiffness
- Infection
- Blood clots (deep vein thrombosis)
- Nerve and blood vessel damage
- Ligament injuries
- Patella (kneecap) dislocation
- Plastic liner wears out
- Loosening of the implant
If you find difficulty in performing simple activities such as walking or climbing stairs because of your severe arthritic knee pain, then total knee replacement may be an option for you. It is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume your normal activities of daily living.
Avoiding Problems after Surgery
Blood clot prevention:
Follow our instructions carefully to minimize the potential of blood clots that can occur during the first several weeks of your recovery.
Warning signs of possible blood clots in your leg include:
- Increasing pain in your calf.
- Tenderness or redness above or below your knee.
- Increasing swelling in your calf, ankle, and foot.
Warning signs that a blood clot has travelled to your lung include:
- Sudden increased shortness of breath.
- Sudden onset of chest pain.
- Localised chest pain with coughing.
Notify your us immediately if you develop any of these signs.
Preventing infection:
The most common causes of infection following total knee replacement surgery are from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your knee replacement and cause an infection.
Following your surgery, you should take antibiotics prior to dental work or any surgical procedure that could allow bacteria to enter your bloodstream.
Warning signs of a possible knee replacement infection are:
- Persistent fever (higher than 100 degrees orally).
- Shaking chills.
- Increasing redness, tenderness, or swelling of the knee wound.
- Drainage from the knee wound.
- Increasing knee pain with both activity and rest.
Notify us immediately if you develop any of these signs.
Avoiding falls:
A fall during the first few weeks after surgery can damage your new knee and may result in a need for further surgery. Stairs are a hazard until your knee is strong and mobile. You should use a cane, crutches, a walker, handrails, or someone to help you until you have improved your balance, flexibility, and strength.
We will help you decide what assistive aides will be required following surgery and when those aides can safely be discontinued.
How your new knee is different?
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending activities. Improvement of knee motion is a goal of total knee replacement, but restoration of full motion is uncommon. The motion of your knee replacement after surgery is predicted by the motion of your knee prior to surgery. Most patients can expect to nearly fully straighten the replaced knee and to bend the knee sufficiently to go up and down stairs and get in and out of a car. Kneeling is usually uncomfortable, but it is not harmful. Occasionally, you may feel some soft clicking of the metal and plastic with knee bending or walking. These differences often diminish with time and most patients find these are minor, compared to the pain and limited function they experience prior to surgery.
Your new knee may activate metal detectors required for security in airports and some buildings. Tell the security agent about your knee replacement if the alarm is activated.
After surgery, make sure you also do the following:

- Participate in regular light exercise programs to maintain proper strength and mobility of your new knee.
- Take special precautions to avoid falls and injuries. Individuals who have undergone total knee replacement surgery and suffer a fracture may require more surgery.
- Notify your dentist that you had a knee replacement. You should be given antibiotics before all dental surgery for at least 3 months’ post operatively.
- Please see us periodically for a routine follow up examination and X-rays.
It is important that you contact our office directly after discharge if you have any concerns whatsoever about your operation and progress. We will always be available to answer any queries.
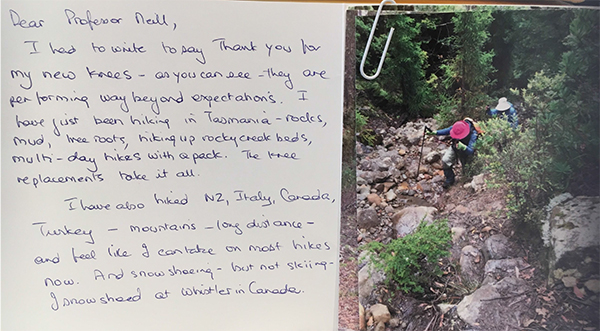
Patient Feedback
Patient 17 years after TKR climbs Mt Kiliminjaro

- Is Simultaneous Bilateral Total Knee Arthroplasty (BTKA) as Safe as Staged BTKA?
- Total Knee Replacement Anaesthesia
All the Patient Forms are Adobe PDF files and require an Adobe Acrobat Reader If you do not have a copy, you can obtain a free copy of the Reader from the Adobe site. Click on the Adobe logo below go download the Adobe Reader.





