Total Hip Replacement
Direct Anterior Total Hip Replacement using MAKO Robotic technology by Dr Amir Kalanie
Total hip replacement is a surgical procedure in which the damaged cartilage and bone is removed from the hip joint and replaced with artificial components. The hip joint is one of the body's largest weight-bearing joints, located between the thigh bone (femur) and the pelvis (acetabulum). It is a ball and socket joint in which the head of the femur is the ball and the pelvic acetabulum forms the socket. The joint surface is covered by a smooth articular cartilage which acts as a cushion and enables smooth movements of the joint.
A number of diseases and conditions can cause damage to the articular cartilage. Total hip replacement surgery is an option to relieve severe arthritis pain that limits your daily activities.
Disease Overview
There is currently no medical cure for arthritis. All non-operative therapies aim to manage the disease and relieve symptoms. Joint replacement surgery is the only real cure for arthritis. Patient with two artificial knees and hips for osteoarthritis.
Arthritis is inflammation of the joints resulting in pain, swelling, stiffness and limited movement. Hip arthritis is a common cause of chronic hip pain and disability. The three most common types of arthritis that affect the hip are:
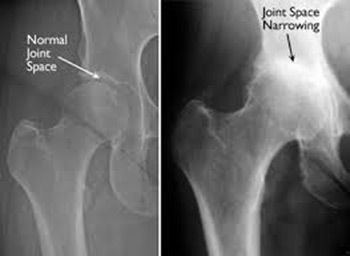
- Osteoarthritis: It is characterised by progressive wearing away of the cartilage of the joint. As the protective cartilage wears down, the bone ends rub against each other and cause pain in the hip.
- Rheumatoid arthritis: This is an autoimmune disease in which the tissue lining the joint (synovium) becomes inflamed, resulting in the production of excessive joint fluid (synovial fluid). This leads to loss of cartilage causing pain and stiffness.
- Traumatic arthritis: This is a type of arthritis resulting from a hip injury or fracture. Such injuries can damage the cartilage and cause hip pain and stiffness over a period of time.
What medications should I stop before operation?
Many tablets can cause excessive bleeding at operation so it is essential to cease taking the medication well beforehand. However, if you are taking such medication for problems with your heart or blood vessels, please ensure you discuss this with A/Prof Neil.
Stop the following one month (30 days) prior to admission:
HRT (excluding Prednisone), Tamoxifen, Arava, Letrozole
Stop the following 5 days prior to admission:
Alka-Seltzer, Asasantin, A.S.A., Aspirin, Aspalgin, Aspro Clear, Asprodeine, Soluble, Astrix, Bex, Bufferin, Cartia, Cardiprin, Clusinol, Chemgesic, Codiphen, Forte,Clopidogrel, Coois, Codox, Codral Forte, Disprin, Doloxene, Ectorin, Ensalate, Iscover, Morphalgin, Orthoxical Cold & Flu Tablets, Percoden, Persantin, Plavix, Rheumat-ese, Rhusal, Solocode, Solvin, Solprin, Salicylamide, SRA, Vincents powder/tabs, Winsprin ANTI-INFLAMMATORY DRUGS, ACT-3, Aclin, Actiprofen, Advil, Arthexin, Arthrotec, Brufen, Bugesic, Candyl, Celebrex, Clinoril, Crysanal, Dinac, Doloboid, Feldene, Fenac, Flexin, Ibuprofen, Indocid, Inflam, Inza, Mefic, Methotrexate, Mobic, Naprogesic, Naprosyn, Nurofen, Orudis, Oruvail, Ponstan, Priohexal, Prioxicam, Proxen, Rafen, Rheumacin, Surgam, Tilcotil, Toradol, Tri-profen, Voltaren ANTICOAGULANTS Warafin/Coumarin/Marevan cease 5 days pre-op.
The tablets will have to be withdrawn prior to surgery and CLEXANE injections are substituted up to the time of operation. ANTICOAGULANT tablets will be resumed after surgery under the direction of A/Prof Neil.
HERBAL MEDICINE Arnika, Echinacea, Fish Oil, Garlic (7 Days), Ginger, Ginseng (7 Days), Gingko (36 Hours), Krill Oil, Primrose Oil, Saw Palmetto, Vitamin E
PANADOL, PANADEINE OR PAINKILLERS may be taken for pain relief up to the time of operation
If you are uncertain about any of your medications, please discuss this with A/Prof Neil or Staff
What is Arthritis
What is Hip Arthritis?
A painful stiff hip can keep you from doing simple things in life, even walking without pain. Total hip replacement is often indicated when the cause of pain is from arthritis of the hip joint. In this operation, your arthritic painful hip is replaced with an artificial device or “prosthesis”. Total hip replacement is a safe, effective and reliable operation that can relieve your hip pain and return you to most of the activities that you enjoy. Nowadays the prosthesis should last 25 years or more.
The bone ends in a joint, such as the hip or knee, are covered with a smooth glistening material called cartilage. This material cushions the underlying bone from excessive force or pressure and allows the joint to move easily without pain.
In Osteoarthritis (OA), the cartilage becomes worn and no longer allows smooth movement of the joint. The bone surfaces may begin to rub together in more advanced disease causing severe pain, swelling and stiffness in the affected joint, particularly if the joint bears weight.
The hip joint may also be damaged by Rheumatoid Arthritis, where the lining of the joint produces destructive enzymes that eat away at cartilage, bone and tendons.
Trauma such as a fracture through the hip or a dislocation can cause permanent damage to the cartilage producing arthritis.
Avascular Necrosis (AVN) is when the blood supply to the ball of the hip joint is lost, for one of many reasons, and can result in death of the bone with collapse of the hip joint causing severe pain and limp.
Total hip replacement can relieve pain and improve function in all these conditions.
What type of hip replacements are there, and which one is best for me?
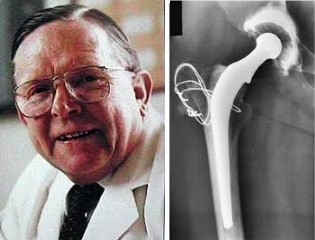
Total Hip Replacement (THR) is one of the greatest medical advances of the 20th century and was pioneered by Sir John Charnley in the 60’s in Wrightington, England. His original prosthesis (on the right) was a simple stainless steel stem and plastic shell cemented in the bone and carried out by removing the gluteal muscles with bone and rewiring them. This was the “gold standard” in THR for many ears, but there have been significant advances since then, both in materials and surgical technique.
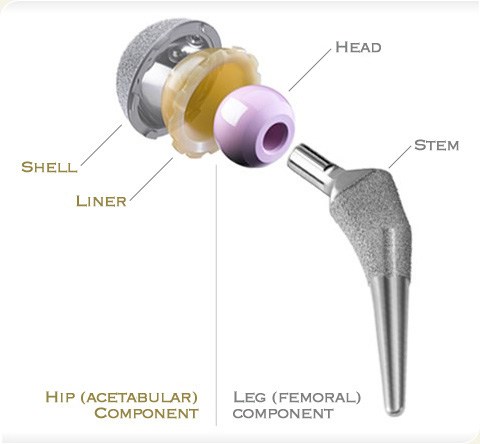
Your hip is a ball-and-socket joint where the thigh bone articulates with the pelvic bone. Your hip prosthesis has the same basic parts as your own hip joint. A ball, either metal or ceramic, is used to replace the worn ball of the thigh bone, with a stem inserted into the tube of the bone to anchor the prosthesis to your femur. A socket, either cemented plastic or press-fit titanium with a ceramic or plastic liner, is implanted into your worn socket in the pelvic bone.
Like a healthy hip, your prosthesis has smooth gliding surfaces that allow the joint to move easily without pain. The bearing surfaces are either metal or plastic, ceramic on plastic, or ceramic on ceramic as seen bottom right. Each has advantages and disadvantages. Ceramic/ceramic is without doubt the superior bearing in terms of lasting, but is less forgiving and has to be implanted in perfect position.
Hard on hard bearings (metal/metal or ceramic/ceramic) became popular in the late 90’s. Unfortunately, metal/metal articulations have had an unacceptably high failure rate due to the production of metal wear particles in the hip and the bloodstream, so called “metallosis”. Many have been withdrawn from the market by the manufacturers, and patients re-operated.

Importantly, at STVBJ, we have been using non-cemented prostheses routinely in ALL patients combined with hard on hard ceramic bearings since 1998.
The porous implants become “osseo integrated” where the bone bonds to it. Revision of ceramic hips for wear or “osteolysis” is virtually unheard of, and we have not experienced “sueaks” or fracture of ceramic as reported occasionally in the literature.
The ceramic is virtually frictionless and wear studies suggest a life of about 30 years.
This means most THR’s done with this technology should last for life, a very exciting prospect!!

Biolox Delta
3rd generation ceramic hip bearing CERAMTEC, Germany.
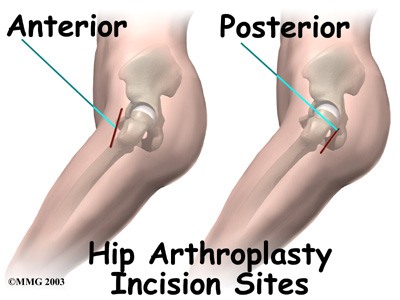
Which surgical approach is better: mini-posterior or anterior?
Posterior approach for THR has been the most widely utilised throughout the world for many years. Recently there has been renewed interest in a very old surgical approach called the “Smith Petersen” relabelled as the Direct Anterior Approach (DAA) or “Intermuscular Approach”. This has been purported to allow faster patient recovery because “no muscles are cut”. The evidence for this being a “superior” approach to the more utilised “mini posterior” approach is sparse and anecdotal, and heavily tainted by conflict of interest.
DAA has been pushed commercially by various Orthopaedic Companies by direct marketing to General Practitioners as being a superior operation performed by only “expert “surgeons.
A recent very good comparative study from the Mayo Clinic found NO difference in recovery or outcome between either approach in experienced hands. ("Direct Anterior versus Mini posterior THA with the same Advanced Perioperative Protocols: Surprising Early Clinical Results." Pagnano et al. CORR (2015) 473: 623-631.) There was no difference at 2 hours, 2 days, 2 months and 2 years between patients except that the DAA was more expensive, time consuming, required a traction table and X-ray control, and more difficult to do.There has been no difference in dislocation rate, which is often touted as a reason for the DAA, with most series well below 0.5%, and our practice 0.3%. The recognised "learning curve" for this procedure is about 40 cases with higher documented complications and failures. The consensus amongst non-conflicted surgeons is that high volume surgeons generally have less complications and excellent results, irrespective of the surgical approach used. "If it ain"t broken, then don't fix it" comes to mind.
Furthermore, the view of the Australian Arthroplasty Society (the subspecialist joint replacement group of The Australian Orthopaedic Association, of which A/Professor Neil is a senior member and contributor), is also that volume of surgery by us is the critical factor in outcome after THR, and not the surgical approach.
At St Vincent’s Clinic, the Orthopaedic Department does about 800 joint implant surgeries per annum, of which A/Prof Neil does about 350. We really do have a high volume joint replacement practice, which makes your operation under our care more “routine” and consequently uncomplicated.
At STVBJ both approaches are offered as Dr. Kalanie is a Fellowship trained DAA surgeon, but we would emphasise that the exposure in the DAA is undeniably more difficult, making it a harder operation to get accurate positioning of the implant and restoration of hip mechanics including leg length. It is certainly contra-indicated in obesity. The only immediate advantage appears to be that “hip precautions” are not required in the post-operative period.
Preparing for hip replacement surgery
Hip replacement has become a common and safe procedure -- about 40,000 people in Australia get a new hip each year. Good preparation can speed your recovery after surgery and help ensure a successful result.
Here are some ways to prepare for your hip replacement surgery.
- Learn about the procedure. Before you check into the hospital, learn everything you can about hip replacement surgery, the type of replacement joints available, and the details of recovery. Check out reputable web sites such as the American Academy of Orthopaedic Surgeons (AAOS) or the American Association of Hip and Knee Surgeons (AAHKS) or the Australian Orthopaedic Association, as well as www.stvincentsboneandjoint.com.au
- Write down questions before your consult. You're going to have lots of questions for Dr Neil, but it may be hard to remember them all when you're sitting in the office. Instead, write down questions beforehand on a pad and go in prepared.
- Consider the impact on work. Think through how surgery and recovery will affect your job and home life. Depending on the demands of your job, you may need a few weeks -- or even a few months -- away from work.
- Get in shape. If you go into surgery in good shape, you could dramatically speed up your recovery. If you're overweight, try to lose a few kilos. Building up strength is important too. A strong upper body will make it much easier to get around on crutches or a walker. Some pool or gym work will help.” Prehab” where you do a programme at the rehab unit pre-op is a good idea.
- Meet with a physio therapist. Physio therapy and rehabilitation with hydrotherapy is key to a good recovery and a successful hip replacement. Instead of waiting until after surgery, see if you can meet with the physio therapist now. Learning some of the exercises before surgery could make them easier to do later.
- Test drive your crutches or walker. See if you can borrow a pair of crutches or a walker. Try to get comfortable using them now.
- Get family and friends to help. No one can recover from hip replacement alone. Work out a plan with your family. If you live alone, see if a friend or close relative could stay with you for a while. If you don't have a support system you can rely on, you could stay in a rehab facility (Wolper Jewish Hospital and St Luke's Care) after surgery while you recover. And extended care programme (ECP) is available at St Vincents Private Hospital Sydney.
- Rearrange your home. If you'll be recuperating at home, you need to make changes now. Consider moving your bedroom to the ground floor. Set up a kind of "base camp" where you'll spend most of your time -- with phone, computer, remotes, and everything else you'll need in easy reach. Make sure your house will be easy to move around in with a walker or crutches. Remove possible tripping hazards, such as loose rugs.
- Buy assistive devices. Gadgets -- such as reachers or long-handled shoe horns -- will come in handy after surgery. Setting up railings on stairways or in the bathroom could also make life after surgery easier and safer. Our occupational therapist will help with these at the rehab facility.
Your operation and hospital stay
Total hip replacement is a major operation. It involves admission to hospital, anaesthesia, rehabilitation and well defined risks.
The operation takes us about 90 minutes to perform. It is an operation Dr Neil performs about 150 times per year. This represents a busy surgical practice specialising in hip and knee replacement.
Anaesthesia used is often a spinal block with sedation/general anaesthesia combined with intraoperative injections of local anaesthesia, and a "Pain buster" local anaesthetic catheter which is left in the joint. You will not be aware during the operation. You can be completely asleep if you wish. Your anaesthetist will discuss this with you the night before surgery.
Your operation will be carried out in an orthopaedic operating theatre at St. Vincent’s Private Hospital. Strict aseptic conditions will apply, including the use of full exhaust “space suits”. Your arthritic hip is dislocated surgically and the ball of the femur removed. Drills and reamers are used to prepare the bone surfaces for accurate implantation of your new hip. Special care is taken to ensure the hip is stable and the length of the leg is the same as the other side if possible. The wound is sutured close with a dissolving material so no stitches are seen or need to be removed.
After the operation, you will be transferred to the recovery ward for observation for a period of hours. A check X-ray of your new hip will be taken and shown to me before you return to the hospital ward.
Post-operative programme in hospital
Day 1
You will be encouraged to stand and walk fully weight bearing with a walking frame. You should start a light normal diet if there is no nausea. we start prune juice and other laxatives early, as a lot of the pain killers tend to cause constipation. If you take something regularly normally, you should bring it in to hospital and it will be prescribed. It is not unusual to have a first bowel motion at Day 3 or later.
You will have a drip with fluids and antibiotics running into the vein, an indwelling urinary catheter draining the bladder of urine and a drain in the hip wound draining blood from the operation site. Pain medicine will be given regularly orally for at least 48 hours, and then as required. Calf compressors are applied to decrease clots forming in the legs. Heel Protectors are used to avoid pressure ulcers.
Day 2
If you have been successful in standing and walking a few steps ton Day 1, then all tubes will be removed and your dressing changed today. You may shower if you feel up to it. You will be walked twice today with your physio out of the room.
Day 3, 4
Mobilising twice daily, moving onto crutches or stick. Normal diet and bowel habit. Reducing pain medicine. Can sleep on back or non-operated side (Pillow between legs for mini posterior approach. No “hip precautions” for DAA.
Day 5
Today you will be discharged provided that we feel you are well enough, the wound looks god and there are no medical issues. We do Doppler ultrasound scans routinely on all THR patients prior to discharge. Most patients go to rehab for a week or 2, but some go directly home or to “ECP” (where the physiotherapist visits you at home provided you are in the area.
First 6 weeks
Graduated exercise programme with a walking aid outdoors. Aim to be doing about an hour of something, including walking, pool, exercise bike or gym.
Left THR may drive automatic car at 2 weeks, right THR should wait till 6 weeks. Clinical review at week 6 in Dr Neil’s rooms with x-rays. This appointment will be given to you at time of initial booking for surgery. It would be appreciated if accounts settled at this time as well.
Return to activities/sport?
Once you have undergone a THR, it is your implant for life and you need to look after it to get the longest life from your new joint. You should avoid impact, that is running and jumping, forever. Run in an emergency but not for exercise.
After about 3 months, you can do ALL other activities within reason, including walking, hiking, trekking, swimming, skiing, golf, doubles tennis, cycling, scuba diving, horse riding, etc.
Any activity that has a risk of falling, and therefore trauma to your new hip, you do at your own risk.
Your hip will continue to improve and feel more normal over at least 12 months or longer, by which time we will have done a final check and discharged you if all is well.
For THR, the implant we use is the Global Cup and Paragon Stem (Global Orthopaedic Technology)
Risks
As with any major surgical procedure, there are certain potential risks and complications involved with total hip replacement surgery. The possible complications after total hip replacement include:
- Infection
- Dislocation
- Fracture of the femur or pelvis
- Injury to nerves or blood vessels
- Formation of blood clots in the leg veins
- Leg length inequality
- Hip prosthesis may wear out
- Failure to relieve pain
- Scar formation
- Pressure sores
Severe protrusio with poor bone stock represents very difficult surgery
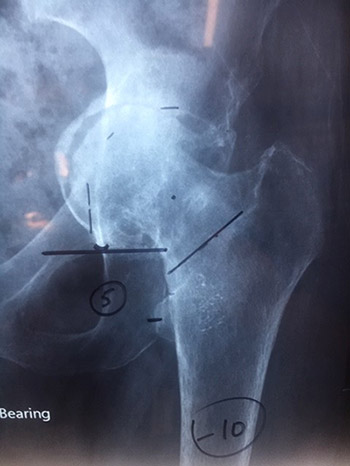
Postoperative Xray following successful operation

X-ray Osteoarthritis Hip
Happy patient 3 months post THR having just completed the Larapinta Trail


Related Links
You will need the Adobe Reader to view and print these documents. 



